Public Service Reform Plan 2014-2016
3.2 Health Sector
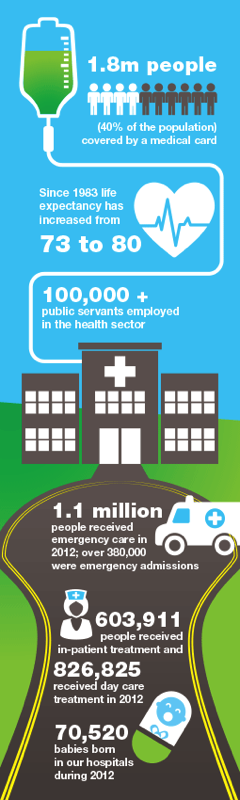
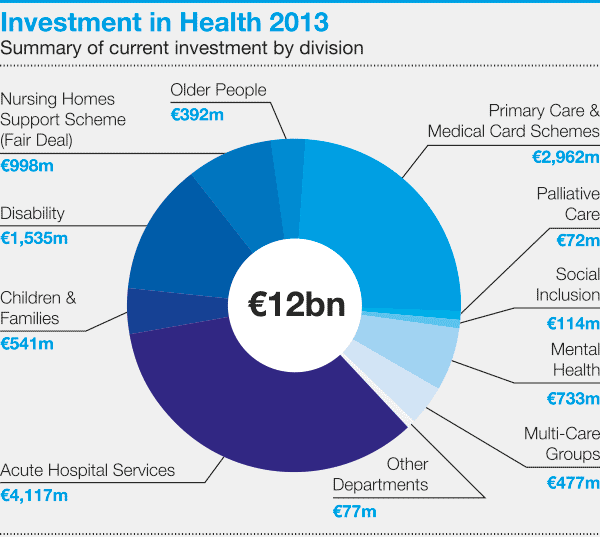
The challenge of ensuring that these reforms are implemented successfully and on target is immense, specifically when considering the need to reduce costs and at the same time deal with increased demands for public services. The financial pressures on the health system make it even more important that comprehensive health reform is introduced. Only in this way can the services people need be delivered, even as the available financial resources diminish. The Health Reform Plan however is fundamentally changing the health service for the better.
One of the key reforms is the development of eHealth, which is about the transfer of health resources and health care by electronic means, including health information, education and training and health management. The use of eHealth will result in greater efficiencies, savings and improved patient care through faster and better diagnosis.
The Future Health programme is built on four key interdependent pillars of reform:
[i] Health and wellbeing: to keep the population healthy rather than just simply treating ill people;
[ii] Service reform: to deliver a new, less hospital focused model of care, which treats patients safely, at the right time, with value for money, with the right service and as close to home as possible. An example of this is how the HSE is working with organisations such as the Genio Trust, a registered charity, to develop new ways of providing services to people in the community, such as people with dementia. It is proposed to expand these projects to include hospitals. The lessons learned will be applied more broadly to the development of health services.
The priority objective is to enable people to age with confidence, security and dignity in their own homes and communities for as long as possible. The Department of Health is currently reviewing the Fair Deal scheme with a view to removing barriers to patients and providing more financial support for home care so that more patients can be maintained in their homes and communities. The Positive Ageing Strategy will support people in maintaining their physical health and wellbeing;
[iii] Structural reform: to implement the steps, including the necessary legal and structural changes to the health system, that will be required to fundamentally shift the model of public health care from a tax-funded system to combination of UHI and tax funding; and
[iv] Financial reform: to ensure that the financing system is based on incentives that are aligned to fairness and efficiency, while reducing costs, improving control and delivering better quality.
Services will be located in order to maximise skills and expertise and to ensure the provision of high quality and safe patient care, appropriate to each hospital.

[i] Performance improvement: to drive improvements in unscheduled care targets and hospital outpatient performance; to reduce maximum waiting times; and develop better information systems, including the unscheduled care information system for hospitals. There are now fewer patients waiting on trolleys in Emergency Departments than in previous years. Work is also continuing to reduce waiting times for adults, children and outpatients;
[ii] Hospital groups: in order to progress implementation of the recommendations of the Hospital Groups report and the Smaller Hospitals Framework, the Department of Health is developing policies to guide overall hospital services reorganisation to ensure a coherent approach to progress hospital group implementation, aimed at achieving the best hospital service nationally. Hospital Groups will provide a more efficient and effective range of health services to the people in their area. Services will be located in order to maximise skills and expertise and to ensure the provision of high quality and safe patient care, appropriate to each hospital.
The hospital groups will facilitate cooperation between academia and industry and will support innovation and collaboration with hospitals to benefit patients in tangible ways such as e-prescribing and enhanced connectivity of patients to their clinicians and their service providers;
[iii] Primary care: access to a universal GP service will be commenced by providing all children aged 5 and under with access to a GP service without fees. Work will continue on the development of options for the provision of a GP service without fees to the entire population by early 2016 as a step towards the introduction of Universal Health Insurance. Since 2011, the Government has progressed 34 Primary Care Centres and a further 12 are approved for building. This infrastructure will have a significant impact on the ability of the primary care system to deliver services nearer to people’s own homes. As resources permit, this network will be expanded.
Medicines management is being given a high priority. Driving down the cost of medicines is a key priority objective. The top 20 medicines, based on cost, will be a key focus and will reduce prices by between 30–70%;
[iv] Universal Health Insurance and Money Follows the Patient: intensive work is continuing on preparing the private health insurance market for UHI and on the many elements that will combine to form a new system of UHI. Work is well advanced on a White Paper on UHI to be published early in 2014.
The traditional funding model based on outturns and budget projections will be phased out and in future, budget allocations will follow the actual care being provided to patients, subject to budgetary limits. The Department of Health and HSE have worked closely to ensure that phased implementation of Money Follows the Patient commenced in January 2014. The new funding model will mean that hospitals will be funded on the basis of the agreed level of services they provide and the number of patients that they treat. Budgetary discipline will be delivered under the new system through the use of fixed budgets for MFTP activity;
[v] Patient safety and quality: the Minister for Health intends that the Patient Safety Agency will be established on an administrative basis, initially within the HSE structures, in 2014. A licensing system for public and private health service providers will also be developed. These will deliver higher quality and safer services for all patients and staff; and
[vi] Health and Wellbeing: “Healthy Ireland” is the national framework for action to improve the health and wellbeing of our country over the coming generation. Healthy Ireland takes a “whole-of-Government” and “whole-of-society” approach to improving health and wellbeing. The vision is for a Healthy Ireland, where everyone can enjoy physical and mental health and wellbeing to their full potential, where wellbeing is valued and supported at every level of society and is everyone’s responsibility.
These reforms will create a fundamentally different model of healthcare that will improve health and wellbeing and provide faster, fairer access to hospital care; free access to GP care for everyone; and better management of chronic illness. These reforms will lead to more people being cared for in their own homes; improved quality and safety; and greater affordability of healthcare.